Please refer to the March 2024 guidance supplement on the SDCEP website for updated MRONJ incidence information.
- Advise the patient that due to medication they are taking, there may be a small risk of developing MRONJ but ensure that they understand that the risk is low.
-
- Explain that MRONJ is typically diagnosed when there is exposed bone in the jaw that has persisted for 8 weeks and can occur spontaneously or after dental treatment that impacts on bone, such as an extraction. Other symptoms include loose teeth, pain, tingling, numbness, altered sensation or swelling
- Inform patients with dental implants placed prior to commencement of drug treatment of the small risk of spontaneous MRONJ at those sites
- Emphasise that MRONJ is an adverse effect of the drug they are taking and is not caused by dental treatment
- Discuss the benefits of anti-resorptive and/or anti-angiogenic drugs with the patient and why it is important that they continue to take the drugs
-
- Anti-resorptive drugs significantly reduce the risk of fractures, and subsequent chronic pain, in patients being treated for osteoporosis
- Anti-angiogenic drugs restrict the growth of tumour blood vessels and are an important part of some cancer treatments. Anti-resorptive drugs reduce bone pain and the risk of fractures in patients being treated for cancer
- Drug holidays to avoid the risk of MRONJ associated with dental care are not recommended because the benefits of taking the drugs to manage the patient’s medical condition are likely to outweigh the small risk of developing MRONJ and, in the case of the bisphosphonates or denosumab, stopping the drug does not eliminate the risk of developing MRONJ
- Discuss the overall risk of MRONJ with the patient, based on the medical condition for which they are being treated, using language that they are able to understand. Stress that the risk is small and that the disease is an adverse effect of the medication and is not caused by dental treatment.
-
- For patients being treated with anti-resorptive or anti-angiogenic drugs for the management of cancer, the risk of MRONJ approximates 1%, (range 0 – 2.3%) which suggests that each patient has a 1 in 100 chance of developing the disease. However, the risk appears to vary based on cancer type and incidence in patients with prostate cancer or multiple myeloma may be higher
- For patients taking anti-resorptive drugs for the prevention or management of non-malignant disease (e.g. osteoporosis, Paget’s disease), the risk of MRONJ approximates 0.1% or less, which suggests that each patient has between a 1 in 1000 and 1 in 10,000 chance of developing the disease
- Patients who take concurrent glucocorticoid medication or those who are prescribed both anti-resorptive and anti-angiogenic drugs to manage their medical condition may be at higher risk
- The incidence of MRONJ after tooth extraction is estimated to be 2.9% in patients with cancer and 0.15% in patients being treated for osteoporosis
The figure below may help you to explain the risk of MRONJ to patients. The frequency is based on the assumption that all included individuals have been exposed to a risk factor, such as a bisphosphonate.
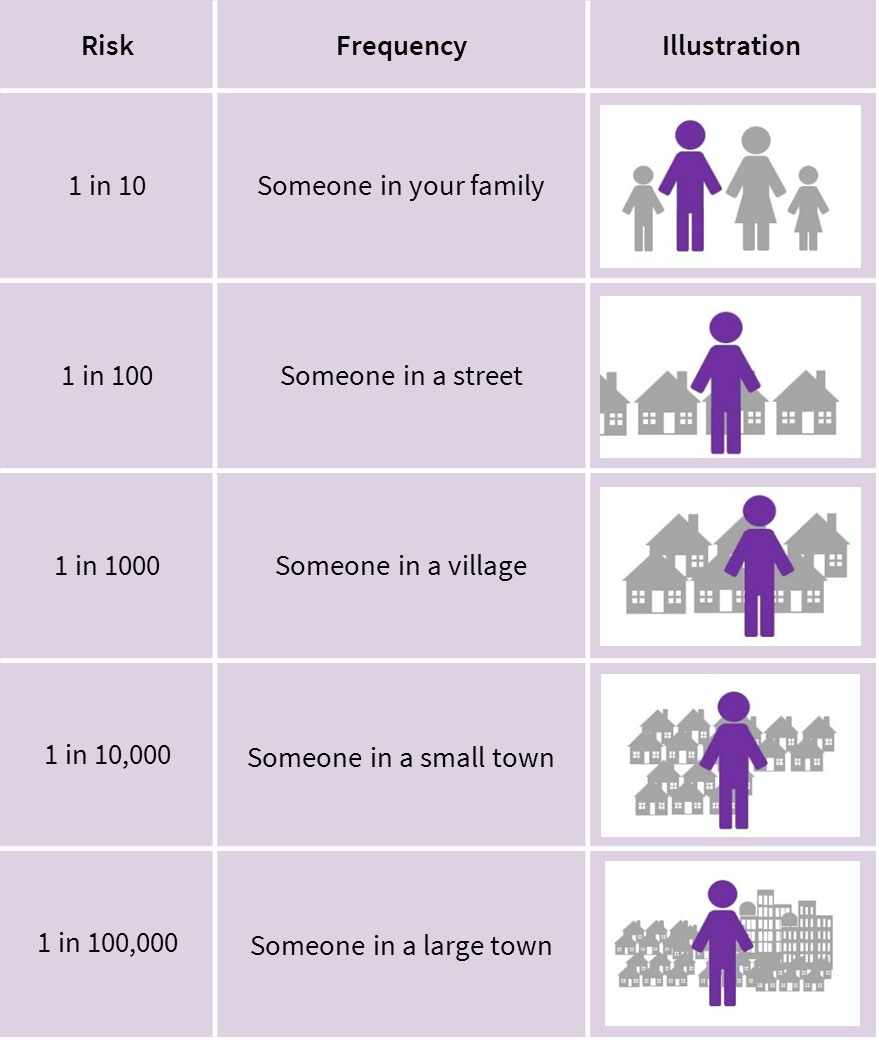
Adapted from Risk Language and Dialects, Calman and Royston, BMJ 1997; 315:939
- Discuss with the patient the steps that they can take to reduce their risk of MRONJ, including improving their oral hygiene and addressing other lifestyle factors such as diet, smoking status and alcohol consumption.
-
- More information on techniques to change patient behaviour can be found in Section 3 of the SDCEP Prevention and Treatment of Periodontal Diseases in Primary Care guidance, including the Oral Hygiene TIPPS behaviour change strategy
- Encourage patients to attend for regular dental checks and to report any spontaneous symptoms such as exposed bone, loose teeth, non-healing sores or lesions, pus or discharge, tingling, numbness, altered sensation, pain or swelling as soon as possible
N.B. Advise patients who are prescribed an oral bisphosphonate not to hold the tablet in the mouth due to risk of damage to the oral mucosa. Advise patients to follow the instructions for administration given by their doctor or pharmacist or as included in the drug information leaflet.
- Discuss with the patient the steps you will take to reduce their risk of MRONJ.
-
- Explain that you will carry out any necessary remedial dental treatment (e.g. extractions, periodontal treatment, refitting appliances or dentures) at an early stage in their medical treatment to ‘future-proof’ their oral health, with the aim of preventing the need for higher risk procedures, such as extractions, in future
- Patients at higher risk from dental caries may also benefit from high fluoride toothpaste or mouthwash
Low Risk Patients
- Inform the patient that although dental treatments that impact on bone, such as extractions, may increase the risk of MRONJ, the risk is still low and the benefits of the dental treatment are likely to outweigh the risks.
- Advise the patient that they will be asked to return after 8 weeks so that you can ensure the extraction socket has healed adequately.
-
- Patients should also be advised to contact the practice at an earlier date if they have any concerns, such as unexpected pain, numbness, altered sensation or swelling in the extraction area
- Low risk patients who consider dental implants should be informed of the risk of MRONJ following the procedure and the small risk of long-term implant failure.
Higher Risk Patients
- Inform the patient that dental treatments that impact on bone, such as extractions, may increase the risk of MRONJ, therefore all possible alternatives should be considered to avoid extractions where possible. However, there will be cases where extraction is the only treatment option.
- If extraction is the most appropriate option, advise the patient that the benefits of the dental treatment are likely to outweigh the risk of developing MRONJ.
- Advise the patient that they will be asked to return after 8 weeks so that you can ensure the extraction socket has healed adequately.
-
- Patients should also be advised to contact the practice at an earlier date if they have any concerns, such as unexpected pain, numbness, altered sensation or swelling in the extraction area
Patients who have exposed bone at 8 weeks or who present with spontaneous MRONJ
- Advise the patient that due to the presence of exposed bone in their jaw, they need to be referred to a specialist for further treatment.
-
- If the patient wishes to know more about the treatment that may be provided in secondary care, advise them that, in general, for cases where only a small amount of bone is exposed treatment may include monitoring, oral hygiene instruction, antibiotics or antibacterial mouth rinses. In cases where a large amount of bone is exposed, surgery may be indicated. However, the treatment they will receive will depend on their individual symptoms and clinical presentation