Patient bleeding risk factors
A patient’s individual risk of bleeding complications is dependent on a variety of factors, including:
- the type and combination of anticoagulants or antiplatelet drugs they are taking
- their underlying health conditions
- other medications that they may be taking
The patient’s medical history and details of the prescribed and non-prescribed medication they are taking should be noted at the start of each course of treatment and checked for any changes at each visit.
There is currently insufficient evidence to directly compare with any certainty the bleeding risks for dental treatment associated with the different anticoagulants and antiplatelet medications.
In clinical trials, incidences of major spontaneous and procedural bleeding events for patients with atrial fibrillation taking dabigatran, apixaban, rivaroxaban or edoxaban were similar or lower than for those taking warfarin.
Estimates from very limited data from dental studies suggest that the risk of post-operative bleeding for dental patients taking DOACs is not significantly different to that for patients on VKAs including warfarin.
Patients who are on dual or combination therapies and are taking more than one anticoagulant or antiplatelet drug are likely to have a higher bleeding risk than those on single drug therapies.
Certain medical conditions are known to be associated with an increased bleeding risk, due to effects on either coagulation or platelet function. These include liver, kidney and bone marrow disorders.
The main conditions affecting coagulation or platelet function which could be relevant for patients also being treated with anticoagulants or antiplatelet drugs are shown in the table below. However, be aware that this is not an exhaustive list.
For medically complex patients such as these, the patient’s general medical practitioner or specialist should be consulted, to establish the extent of the disease in order to assess the likely impact on the bleeding risk for the dental procedure.
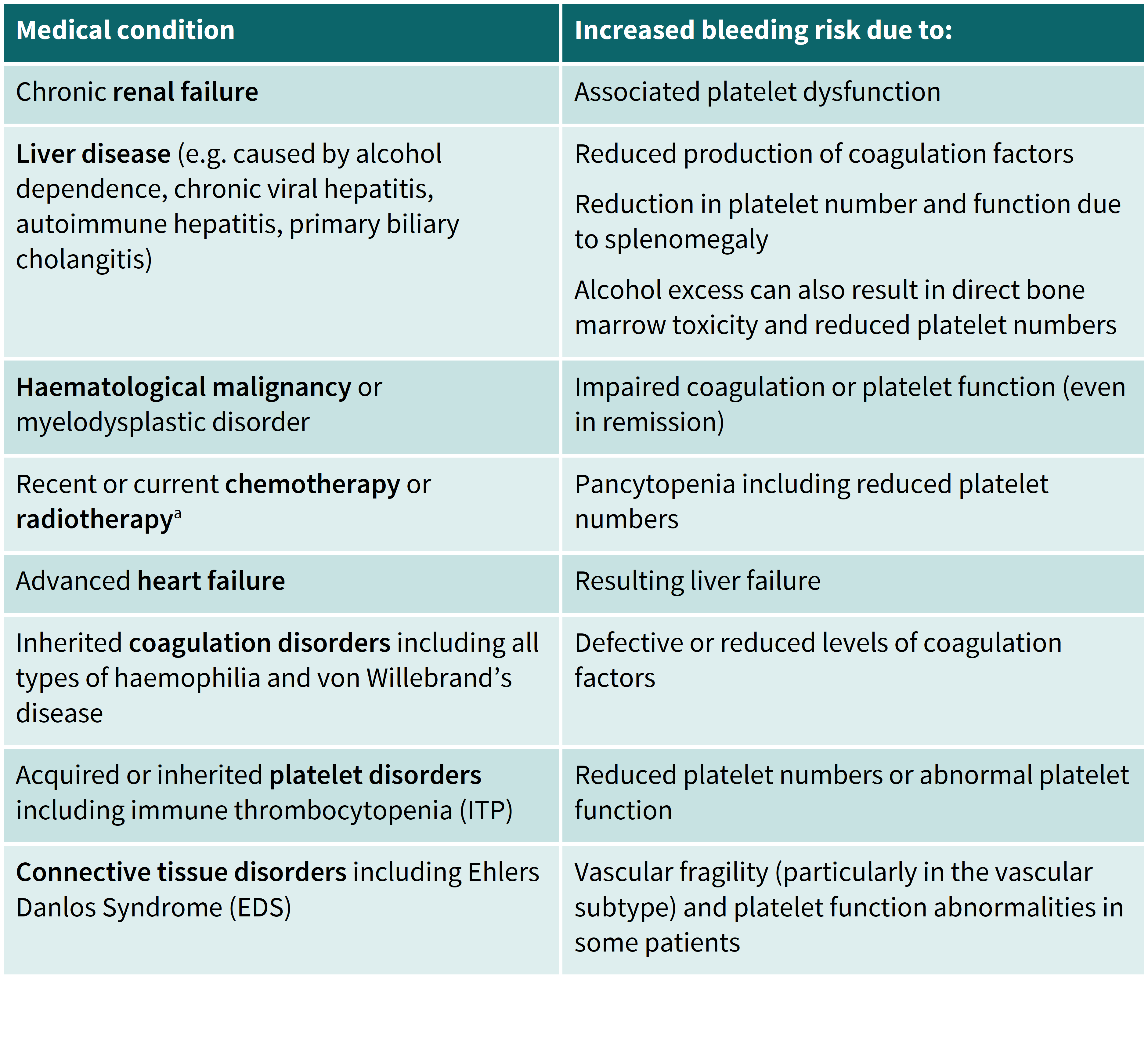
a Have received chemotherapy less than three months ago, or total body irradiation less than six months ago.
A number of different medications can exacerbate a patient’s bleeding risk over and above the effects of the anticoagulants or antiplatelet drugs they are taking.
Although not an exhaustive list, groups of drugs to be aware of include those described in the table below.
For the management of patients taking these additional medications, the patient’s prescribing clinician, specialist or general medical practitioner could be consulted in order to assess the likely impact on bleeding risk.
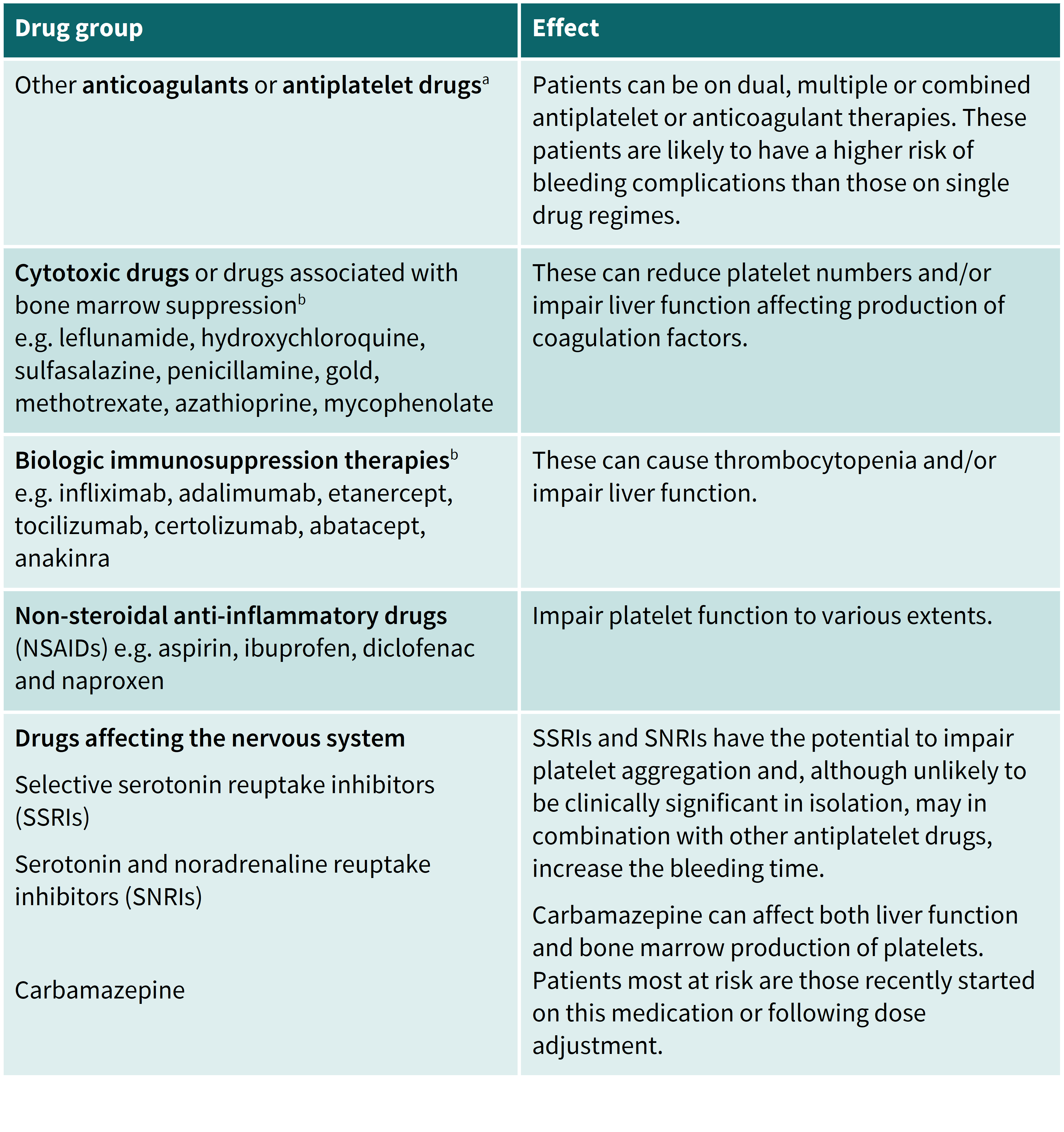
a Be aware that patients may also be taking non-prescribed aspirin, and this antiplatelet agent can in effect convert a prescribed monotherapy into a dual therapy.
b Patients with inflammatory bowel disease or autoimmune/rheumatological conditions are commonly prescribed these drugs.
N.B. Some herbal and complementary medicines may affect bleeding risk, either on their own or when in combination with other anticoagulants or antiplatelet drugs. These include St. John’s Wort, Ginkgo biloba and garlic.